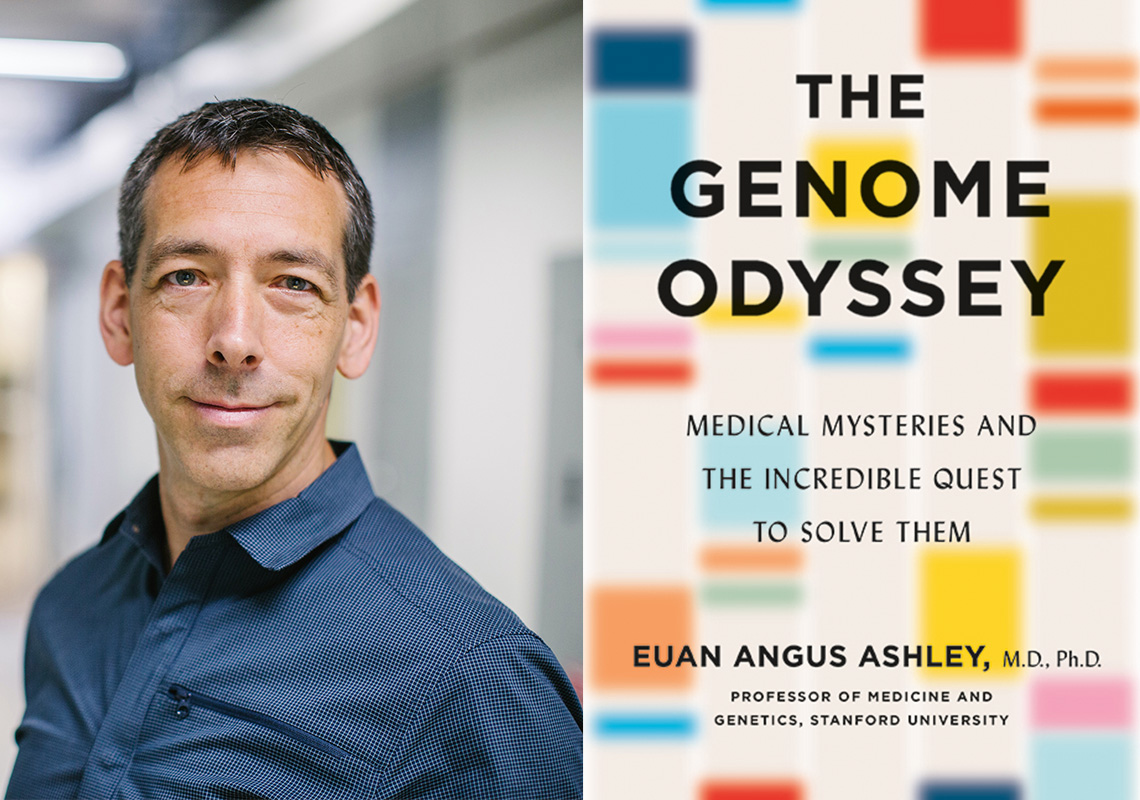
Twenty years ago, the first draft of the human genome sequence was completed. Since then, medical “detectives” like Dr. Euan Angus Ashley have been using the genome to solve their patients’ most puzzling and pressing medical mysteries. And they now understand that this complex and unique data set could be used to prevent disease, from the commonplace to those that cause global pandemics. Celadon Books sat down with Stanford professor of medicine and genetics Dr. Euan Angus Ashley to discuss his book The Genome Odyssey: Medical Mysteries and the Incredible Quest to Solve Them.
Celadon Books: Tell us, what exactly is "genomic and precision medicine"?
Dr. Euan Angus Ashley: Genomic medicine and precision medicine are terms that refer to a new way of understanding disease and treating patients. Precision medicine encapsulates the idea that we can, through the use of modern technology, understand disease at a deeper level and treat it more precisely. Practically, that means some diseases come to be understood as many different diseases, each of which can be addressed with medications that are just right for that group. It is similar to the idea of “personalized” medicine where we try to understand the make-up of each individual, so we can give the treatment that will work best and cause the fewest side effects for them.
The most common technology for helping us more precisely define disease is sequencing the human genome. We have recently witnessed a revolution in our ability to cheaply sequence the human genome with the cost dropping from $3 billion for the first genome (the Human Genome Project, completed in 2001) to around $100 today. This is the equivalent of being able to buy a $400,000 Ferrari for about 1 cent!
Celadon: What has been your team's role in the recent advancements in this field? And why are you the best person to tell this story?
Dr. Ashley: Everyone has his or her own stories! In this book, I tell stories from my team’s work and feature my own patients, but we all stand on the shoulders of so many who came before us.
We realized about a decade ago that, as the price of genome sequencing was dropping, patients would soon have access to their genome information. We also recognized that medicine as it was then practiced was not ready for that size of data. A cholesterol test, for example, is about five numbers, whereas a genome is 6 billion. How do we build for the future of medicine when we need to incorporate data at that scale?
This was what I was thinking when I wandered into the office of a friend and colleague at Stanford in the fall of 2009. He had at that time just become the fifth individual in the world to have his genome sequenced. He showed me his genome on his screen and my jaw dropped. I was used to waiting three months to see the results of sequencing just five genes in my patients. And here he was casually showing me his whole genome (in which the 20,000 genes represent only 2% of the total information!).
As he started telling me about his family history of heart disease and his cousin’s son who had died suddenly at age 17 without known cause, suddenly he became not just my colleague but also my patient. And, at that moment it dawned on us that he was about to become the first patient in the world to walk into a doctor’s office with a genome on a hard drive. And the doctor in question was me. Realizing the scale of the challenge, I rapidly put together a team of Stanford and Harvard colleagues to try to work out how to medically interpret a whole human genome. The question was, how do we bring the entirety of our knowledge of human genetics to bear on the genome of just this one human? Our quest to answer that question and everything that came next is what I describe in the book.
Celadon: You liken the work of doctors and geneticists to the work of a detective. Why is that, and what makes a doctor a good medical detective?
Dr. Ashley: From the earliest days of medical school, we teach our students to be detectives. Patients often present as medical mysteries. We teach these young doctors in training to observe carefully, to gather clues, to examine the scene, to probe the witnesses, and finally solve the case and arrest the culprit! Not many people know that author Arthur Conan Doyle was a physician and that his character Sherlock Holmes was inspired by a surgeon from Edinburgh. There are hundreds of parallels between doctors and detectives in the stories of Sherlock Holmes. I talk about these parallels and those from my own medical practice in the book. I describe patients who have spent years trying to find answers, visiting doctor after doctor, in a long and arduous journey sometimes known as a medical “odyssey” after the Greek tragedy of that name. I describe the efforts of doctors all over the globe who work together to solve these mysteries.
Remarkably, the tools we mostly use — sight, sound, and smell — haven’t changed in thousands of years — until now. Today, we have a much more powerful “magnifying glass” to help us solve medical mysteries: the human genome. In fact, when we study patients with diseases that have escaped all attempts at medical science to solve them, using the genome, we are able to solve them about a third of the time. In many cases, the answer points directly to a medicine that can help.
Celadon: Tell us about one of your patients whose medical journey was dramatically improved by genome sequencing. How did their case change the way you view your work?
Dr. Ashley: One story I tell in the book is of a little girl who, while still in her mother’s womb, was found to have a heart rate about half what it should be. We transferred her mother to Stanford children’s hospital and little Jazlene was born by cesarean delivery shortly after. We realized immediately that her heart rate was low because she had a rare genetic heart disease that was also associated with dangerous heart rhythms. In fact, this little one suffered five cardiac arrests (where the heart stops beating and you need to give CPR) on the first day of her young life. Although we had a label for the syndrome, we realized that this was a syndrome where precision medicine could help (a molecular understanding of the disease would allow us to treat her exact underlying condition), so we decided to sequence her genome.
Normally that would take weeks or months, but she didn’t have that kind of time. We pulled favors from colleagues across academia and industry, biotechnology and the pharmaceutical industry to get her genome sequenced as fast as it had ever been done. A few days later, we found the answer. She had inherited one dangerous gene variant from her mom and one from her dad. Isolated in each parent, these variants caused little harm. Together in their daughter, they caused potentially fatal heart rhythms. Fortunately, because we now understood what was causing her cardiac arrests, we could tailor her treatment specifically to that. Five years later, she is safe, happy, well and enjoying school.
More than any other case, this one convinced me that we had to find a way to move quicker, to sequence and analyze genomes faster, to get answers to patients in time to save their lives. It was also a big part of convincing me of the power of family. Families share so much: towels, toothpaste, t-shirts, and also DNA. Sequencing the immediate and sometimes more distant family offers a massive power boost to our ability to solve medical mysteries.
Celadon: In your book, you invite readers to imagine someday walking into the doctor's office with their genomes in hand. What are the implications of a future where that's possible?
Dr. Ashley: Although we’ve come a long way since the “dawn” of genomic medicine, we are really still only at the end of the beginning. To date, genomes have mostly been used for those with rare disease where one “smoking gun” genetic variant can be found and, in some cases, dramatically alter care for that patient. Although more than one in 10 people in the population harbor a rare disease, for most people the genome has yet to impact their lives. However, that is about to change.
Soon, we will use the genome to help prevent diseases like heart disease, cancer, and diabetes — conditions that come to affect almost everyone. In the near future, your doctor will be able to send for a simple blood or saliva test in order to scan your genome for risks of hundreds of diseases and use that information to make more informed decisions about treating you with cholesterol medication, blood pressure medications, or about the nature and frequency of your cancer screening. Genomic medicine is coming to everyone!
Celadon: In light of the current global pandemic, do you think sequencing the genes of a virus can one day help us treat — or even avoid — an outbreak like the one being experienced today?
Dr. Ashley: The role of sequencing in preventing and managing the current pandemic — and the inevitable future pandemics — is clear. Sequencing viruses or bacteria is incredibly powerful for rapidly identifying the cause of an outbreak, whether it is localized food poisoning from a lettuce plant or a global respiratory pandemic. Sequencing is also the reason we knew early on exactly what kind of virus was causing COVID-19. Sequencing the virus genome helped us understand where the virus came from (for example, which animal it normally lives in) and how the virus mutates as it is passed from human to human.
Sequencing or targeting sections of the virus genome is also the basis of the rapid testing that will be required to allow society to return to normal after lockdown. Beyond the virus itself, we can use genomics to understand why some patients have respiratory failure and end up in the ICU while others don’t even know they are infected. Some patients harbor genetic variants in critical genes in their immune system that make them particularly susceptible or potentially immune to the worst effects of the virus. In the future, we will be able to know who those people are and this should help tailor our response dramatically to the people most at risk, a form of infectious disease precision medicine.
Finally, public health monitoring for early detection of outbreaks (via natural or even weaponized biological threats) is readily achieved by sequencing water and sewage supplies. This will need to be a major focus for our state and federal authorities in the future. In fact, it could be argued that the major difference between our response to the 1918 influenza pandemic and the 2020 pandemic is driven by genomics, which has helped us understand the virus causing the disease, test to help limit the spread, and inform our therapies and vaccines.
Celadon: Where are we today? What have we achieved, and what is the next step?
Dr. Ashley: Genomics has come a long way in the 20 years since the draft sequence of the human genome was completed. Today, patients with rare diseases can have their genome sequenced in most countries and that information can help inform their care and family planning. In the future, we have to make this technology available to whoever needs it wherever they are in the world. Next, we have to make sure that genomic data is shared, so we can connect people with rare diseases all over the world. Then we need to start using the genome to predict which diseases you are at risk for. We will integrate this genome information with knowledge of your environment and your lifestyle. Even your smartphone will have access to information in order to integrate your genetics with your lifestyle data from your smartwatch.
The cost of genome sequencing will continue to fall. In some areas, it is as low as $100. We can also sequence a human genome with a sequencer half the size of a deck of cards. We will also be able to generate that data in hours and even minutes. At this cost and with that kind of portability, sequencing will be used around the world, even in rural parts of the developing world, to help maintain food security and to prevent global pandemics. Better, more individualized care — this is the promise of precision medicine: to define, detect and defeat disease.